Enhancement of opioid-mediated analgesia: A solution to the enigma of placentophagia
Mark B. Kristal
Source: Neuroscience & Biobehavioral Reviews Volume 15, Issue 3, Autumn 1991, Pages 425–435
Department of Psychology, State University of New York at Buffalo, Buffalo, NY 14260, USA
Two major consequences of placentophagia, the ingestion of afterbirth materials that occurs usually during mammalian parturition, have been uncovered in the past several years. The first is that increased contact, associated with ingesting placenta and amniotic fluid from the surface of the young, causes an accelerated onset of maternal behavior toward those young. The second, which probably has importance for a broader range of mammalian taxa than the first, is that ingestion of afterbirth materials produces enhancement of ongoing opioid-mediated analgesia. The active substance in placenta and amniotic fluid has been named POEF, for Placental Opioid-Enhancing Factor. Recent research on both consequences is summarized, with particular attention to POEF, the generalizability of the enhancement phenomenon, its locus and mode of action, and its significance for new approaches to the management of pain and addiction.
http://www.sciencedirect.com/science/article/pii/S0149763405800351
Baby blues – postpartum depression attributed to low levels of corticotropin-releasing hormone after placenta is gone
Many new mothers feel depressed for weeks after giving birth. Physicians have vaguely attributed this malaise to exhaustion and to the demands of motherhood. But a group of researchers at the National Institutes of Health has found evidence for a more specific cause of postpartum blues. New mothers, the researchers say, have lower than normal levels of a stress-fighting hormone that earlier studies have found helps combat depression.
When we are under stress, a part of the brain called the hypothalamus secretes corticotropin-releasing hormone, or CRH. Its secretion triggers a cascade of hormones that ultimately increases the amount of another hormone – called cortisol – in the blood. Cortisol raises blood sugar levels and maintains normal blood pressure, which helps us perform well under stress. Normally the amount of cortisol in the bloodstream is directly related to the amount of CRH released from the hypothalamus. That’s not the case in pregnant women.
During the last trimester of pregnancy, the placenta secretes a lot of CRH. The rise is so dramatic that CRH levels in the maternal bloodstream increase threefold. “We can only speculate,” says George Chrousos, the endocrinologist who led the NIH study, “but we think it helps women go through the stress of pregnancy, labor, and delivery.”
But what happens after birth, when the placenta is gone? Chrousos and his colleagues monitored CRH levels in 17, women from the last trimester to a year after they gave birth. All the women had low levels of CRH – as low as seen in some forms of depression – in the six weeks following birth. The seven women with the lowest levels felt depressed.
Chrousos suspects that CRH levels are temporarily low in new mothers because CRH from the placenta disrupts the feedback system that regulates normal production of the hormone. During pregnancy, when CRH levels are high in the bloodstream, the hypothalamus releases less CRH. After birth, however, when this supplementary source of CRH is gone, it takes a while for the hypothalamus to get the signal that it needs to start making more CRH.
“This finding gives reassurance to people that postpartum depression is a transient phenomenon,” says Chrousos. “It also suggests that there is a biological cause.”
COPYRIGHT 1995 Discover
COPYRIGHT 2004 Gale Group
Interactions between the Hypothalamic-Pituitary-Adrenal Axis and the Female Reproductive System: Clinical Implications
George P. Chrousos, MD; David J. Torpy, MB, BS; and Philip W. Gold, MD
Ann Intern Med. 1998;129:229-240.
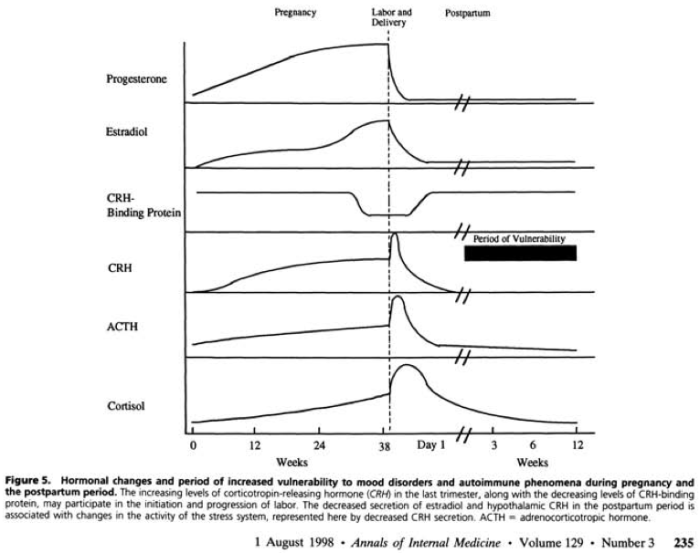
“The clinical implications of placental CRH extend beyond pregnancy, labor, and delivery (76, 77) (Figures 5 and 6). The postpartum period is characterized by an increased incidence of psychiatric and autoimmune manifestations. Indeed, the “post-partum blues,” a mild form of transient depression, occurs in 60% to 70% of women; full-blown post-partum depression affects about 10%; and very severe postpartum psychosis affects about 1 in 1000.
We hypothesized that the postpartum period might be associated with low hypothalamic CRH secretion, which would predispose patients to atypical depression and autoimmune phenomena. We prospectively studied 17 pregnant women who were healthy and had no personal or family history of depression (77). Psychometric testing was done serially beginning with the 20th week of pregnancy and continuing up to a year postpartum. We did ovine CRH stimulation tests at 3, 6, and 12 weeks postpartum. Nine women had normal affect throughout, but 7 developed postpartum blues and 1 developed full-fledged postpartum depression. Plasma levels of ACTH before and after ovine CRH showed little response at 3 weeks, a better but still suppressed response at 6 weeks, and an almost normal response at 12 weeks. Cortisol levels remained in the upper normal range throughout, mostly be- cause plasma cortisol-binding globulin levels were about twice the normal level at 3 weeks, and it took about 3 months or longer for them to decrease to within the normal range. When we separated the women at 3, 6, and 12 weeks into those with the blues or depression and those without a mood disorder, the former had marked suppression of the ACTH response to ovine CRH compared with the latter. Thus, whereas the overall data showed a transient suppression of hypothalamic CRH secretion in the postpartum period, women with the blues or depression had a more severe suppression that lasted longer.
In the postpartum state, the major source of CRH and estrogen, the placenta, is no longer present, whereas the hypothalamic CRH neuron is probably suppressed as a result of previous exposure to high levels of Cortisol for more than 3 months and because of concurrent estrogen deficiency.”
Conclusion: “Placental CRH drives the pituitary-adrenal axis to produce high Cortisol secretion during the latter part of pregnancy. Withdrawal of placental CRH after delivery provokes a secondary hypothalamic CRH deficiency with varying consequences for mood disorders and autoimmune phenomena.
Several lines of evidence suggest that the lethargy, fatigue, hypersomnia, and hyperphagia of atypical depression are associated with hyposecretion of CRH (3). This hyposecretion may contribute to a significant increase in the incidence of allergic and autoimmune phenomena in this form of depression and in its two homolog transient states, the postpartum blues or depression and the postcure state of patients with the Cushing syndrome (48, 77, 79).”
Click to access Interactions-between-the-Hypothalamic-Pituitary-Adrenal-Axis-and-the-Female-Reproductive-System-Clinical-Implications.pdf
Have we forgotten the significance of postpartum iron deficiency?
Bodnar LM, Cogswell ME, McDonald T.
Source: Am J Obstet Gynecol. 2005 Jul;193(1):36-44.
Magee Women’s Research Institute and Department of Obstetrics, Gynecology, and Reproductive Sciences, University of Pittsburgh School of Medicine, PA 15261, USA. bodnar@edc.pitt.edu
The postpartum period is conventionally thought to be the time of lowest iron deficiency risk because iron status is expected to improve dramatically after delivery. Nonetheless, recent studies have reported a high prevalence of postpartum iron deficiency and anemia among ethnically diverse low-income populations in the United States. In light of the recent emergence of this problem in the medical literature, we discuss updated findings on postpartum iron deficiency, including its prevalence, functional consequences, risk factors, and recommended primary and secondary prevention strategies. The productivity and cognitive gains made possible by improving iron nutriture support intervention. We therefore conclude that postpartum iron deficiency warrants greater attention and higher quality care.
http://www.ncbi.nlm.nih.gov/pubmed/16021056
Iron supplementation for unexplained fatigue in non-anaemic women: double blind randomised placebo controlled trial.
Verdon F, Burnand B, Stubi CL, Bonard C, Graff M, Michaud A, Bischoff T, de Vevey M, Studer JP, Herzig L, Chapuis C, Tissot J, Pécoud A, Favrat B.
Source: BMJ. 2003 May 24;326(7399):1124.
General Practice Unit, University of Lausanne, rue du Bugnon 44, 1011 Lausanne, Switzerland.
OBJECTIVE: To determine the subjective response to iron therapy in non-anaemic women with unexplained fatigue.
DESIGN: Double blind randomised placebo controlled trial.
SETTING: Academic primary care centre and eight general practices in western Switzerland.
PARTICIPANTS: 144 women aged 18 to 55, assigned to either oral ferrous sulphate (80 mg/day of elemental iron daily; n=75) or placebo (n=69) for four weeks.
RESULTS: 136 (94%) women completed the study. Most had a low serum ferritin concentration; <or= 20 microg/l in 69 (51%) women. Mean age, haemoglobin concentration, serum ferritin concentration, level of fatigue, depression, and anxiety were similar in both groups at baseline. Both groups were also similar for compliance and dropout rates. The level of fatigue after one month decreased by -1.82/6.37 points (29%) in the irongroup compared with -0.85/6.46 points (13%) in the placebo group (difference 0.95 points, 95% confidence interval 0.32 to 1.62; P=0.004). Subgroups analysis showed that only women with ferritin concentrations <or= 50 microg/l improved with oral supplementation.
CONCLUSION: Non-anaemic women with unexplained fatigue may benefit from iron supplementation. The effect may be restricted to women with low or borderline serum ferritin concentrations.
http://www.ncbi.nlm.nih.gov/pubmed?term=verdon%20iron%20supplementation
The impact of fatigue on the development of postpartum depression.
Corwin EJ, Brownstead J, Barton N, Heckard S, Morin K.
Source: J Obstet Gynecol Neonatal Nurs. 2005 Sep-Oct;34(5):577-86.
College of Nursing, The Ohio State University, 1585 Neil Avenue, Columbus, OH 43210, USA. corwin.56@osu.edu
Previous research suggests early postpartum fatigue (PPF) plays a significant role in the development of postpartum depression (PPD). Predicting risk for PPD via early identification of PPF may provide opportunity for intervention.
Conclusions: Fatigue by Day 14 postpartum was the most predictive variable for symptoms of PPD on Day 28 in this population.
http://www.ncbi.nlm.nih.gov/pubmed/16227513
Maternal iron deficiency anemia affects postpartum emotions and cognition.
Beard JL, Hendricks MK, Perez EM, Murray-Kolb LE, Berg A, Vernon-Feagans L, Irlam J, Isaacs W, Sive A, Tomlinson M.
Source: J Nutr. 2005 Feb;135(2):267-72.
Department of Nutritional Sciences, The Pennsylvania State University, University Park, PA 16802, USA. jbeard@psu.edu
The aim of this study was to determine whether iron deficiency anemia (IDA) in mothers alters their maternal cognitive and behavioral performance, the mother-infant interaction, and the infant’s development. This article focuses on the relation between IDA and cognition as well as behavioral affect in the young mothers. This prospective, randomized, controlled, intervention trial was conducted in South Africa among 3 groups of mothers: nonanemic controls and anemic mothers receiving either placebo (10 microg folate and 25 mg vitamin C) or daily iron (125 mg FeS0(4), 10 microg folate, 25 mg vitamin C). Mothers of full-term normal birth weight babies were followed from 10 wk to 9 mo postpartum (n = 81). Maternal hematologic and iron status, socioeconomic, cognitive, and emotional status, mother-infant interaction, and the development of the infants were assessed at 10 wk and 9 mo postpartum. Behavioral and cognitive variables at baseline did not differ between iron-deficient anemic mothers and nonanemic mothers. However, iron treatment resulted in a 25% improvement (P < 0.05) in previously iron-deficient mothers’ depression and stress scales as well as in the Raven’s Progressive Matrices test. Anemic mothers administered placebo did not improve in behavioral measures. Multivariate analysis showed a strong association between iron status variables (hemoglobin, mean corpuscular volume, and transferrin saturation) and cognitive variables (Digit Symbol) as well as behavioral variables (anxiety, stress, depression). This study demonstrates that there is a strong relation between iron status and depression, stress, and cognitive functioning in poor African mothers during the postpartum period.
http://www.ncbi.nlm.nih.gov/pubmed/15671224
Effects of placentophagy on serum prolactin and progesterone concentrations in rats after parturition or superovulation.
Blank MS, Friesen HG.
J Reprod Fertil. 1980 Nov;60(2):273-8.
In rats that were allowed to eat the placentae after parturition concentrations of serum prolactin were elevated on Day 1 but concentrations of serum progesterone were depressed on Days 6 and 8 post partum when compared to those of rats prevented from eating the placentae. In rats treated with PMSG to induce superovulation serum prolactin and progesterone values were significantly (P < 0.05) elevated on Days 3 and 5 respectively, after being fed 2 g rat placenta/day for 2 days. However, feeding each rat 4 g placenta/day significantly (P < 0.02) lowered serum progesterone on Day 5. Oestrogen injections or bovine or human placenta in the diet had no effect. The organic phase of a petroleum ether extract of rat placenta (2 g-equivalents/day) lowered peripheral concentrations of progesterone on Day 5, but other extracts were ineffective. We conclude that the rat placenta contains orally-active substance(s) which modify blood levels of pituitary and ovarian hormones.
Placenta for Pain Relief:
Placenta ingestion by rats enhances y- and n-opioid antinociception, but suppresses A-opioid antinociception
Jean M. DiPirro*, Mark B. Kristal
Behavioral Neuroscience Program, Department of Psychology, University at Buffalo, Buffalo, NY 14260, USA. dipirrjm@buffalostate.edu 2004
Ingestion of placenta or amniotic fluid produces a dramatic enhancement of centrally mediated opioid antinociception in the rat. The present experiments investigated the role of each opioid receptor type (A, y, n) in the antinociception-modulating effects of Placental Opioid-Enhancing Factor (POEF—presumably the active substance). Antinociception was measured on a 52 jC hotplate in adult, female rats after they ingested placenta or control substance (1.0 g) and after they received an intracerebroventricular injection of a y-specific ([D-Pen2,D-Pen5]enkephalin (DPDPE); 0, 30, 50, 62, or 70 nmol), A-specific ([D-Ala2,N-MePhe4,Gly5-ol]enkephalin (DAMGO); 0, 0.21, 0.29, or 0.39 nmol), or n-specific (U-62066; spiradoline; 0, 100, 150, or 200 nmol) opioid receptor agonist. The results showed that ingestion of placenta potentiated y- and n-opioid antinociception, but attenuated A-opioid antinociception. This finding of POEF action as both opioid receptor-specific and complex provides an important basis for understanding the intrinsic pain-suppression mechanisms that are activated during parturition and modified by placentophagia, and important information for the possible use of POEF as an adjunct to opioids in pain management.
http://www.ncbi.nlm.nih.gov/pubmed?term=placenta%20pain%20dipirro%20kristal
Placentophagia: A Biobehavioral Enigma
KRISTAL, M. B. NEUROSCI. BIOBEHAV. REV. 4(2) 141-150, 1980.
Although ingestion of the afterbirth during delivery is a reliable component of parturitional behavior of mothers in most mammalian species, we know almost nothing of the direct causes or consequences of the act. Traditional explanations of placentophagia, such as general or specific hunger, are discussed and evaluated in light of recent experimental results. Next, research is reviewed which has attempted to distinguish between placentophagia as a maternal behavior and placentophagia as an ingestive behavior. Finally, consequences of the behavior, which may also be viewed as ultimate causes in an evolutionary sense, are considered, such as the possibility of beneficial effects on maternal behavior or reproductive competence, on protection against predators, and on immunological protection afforded either the mother or the young.
Click to access Kristal_biobehavioral.pdf
Placenta increases milk supply
Soykova-Pachnerova E, et. al.(1954). Gynaecologia 138(6):617-627.
An attempt was made to increase milk secretion in mothers by administration of dried placenta per os. Of 210 controlled cases only 29 (13.8%) gave negative results; 181 women (86.2%) reacted positively to the treatment, 117 (55.7%) with good and 64 (30.5%) with very good results. It could be shown by similar experiments with a beef preparation that the effective substance in placenta is not protein. Nor does the lyofilised placenta act as a biogenic stimulator so that the good results of placenta administration cannot be explained as a form of tissue therapy per os. The question of a hormonal influence remains open. So far it could be shown that progesterone is probably not active in increasing lactation after administration of dried placenta.
This method of treating hypogalactia seems worth noting since the placenta preparation is easily obtained, has not so far been utilized and in our experience is successful in the majority of women.
Click to access placenta_lactagogon1.pdf